Temporomandibular joint disorders (TMD)
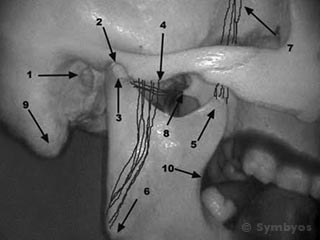
Figure 1: Anatomical structures in and around the temporomandibular joints (TMJs).
The jaw joints are known as the temporomandibular joints (TMJ), so named because they are the point where the temporal bone of the skull, and the mandible (lower jaw) interface. Dysfunction in the joints (TMD) includes clicking, popping, locking and grating. Each of these represents a different step along a continuous pathway of successively more-serious problems. At each step along the pathway, there may be various degrees of pain, or no pain at all.
Anatomical structures (See Figure 1)
- External Auditory Meatus, or earhole
- Glenoid Fossa, the socket into which the condyle of the mandible rests
- Condyle of mandible, a football-shaped bony projection on which the mandible pivots and slides
- Zygomatic Arch, a bridge of bone along which the masseter closing muscles attach
- Coronoid Process of the mandible, to which fibers of the temporalis muscle attach
- Angle of mandible, to which the masseter closing muscles attach
- Anterior temporalis muscle fibers, which are involved in closing the mandible
- Attachment point of the lateral pterygoid muscle, which moves the mandible forward
- Mastoid process of the temporal bone, where muscles that turn the head attach
- Coronoid notch of the mandible, an important landmark for dental injections
A Brief Description of TMJ Function
Major structures in and around the temporomandibular joint (TMJ) are shown in Figure 1. When slightly open, the condyle (3) of the lower jaw (mandible), is resting in the glenoid fossa (2), a concave depression in the temporal bone of the skull base. These are the two bony elements of the joint. In health, there is a cushioning disk between these two bones, which is attached to, and moves with the condyle. It is held in place by a fibrous joint capsule containing synovial fluid.
(1) shows the external auditory meatus (earhole), an important structure because it lies so close to the joint. Sometimes TMJ pain can be felt as ear pain. (4) shows the zygomatic arch, where the masseter muscle (one of the large closing muscles of the jaw) attaches. The other end attaches at the angle of the mandible (6).
Also involved in closing the jaw are the anterior fibers of the temporalis muscle, which attach at (7) and (5), the latter of which is the coronoid process of the mandible. The posterior temporalis muscle fibers move the mandible posteriorly (retrusion).
At (8), muscle fibers of the lateral pterygoid muscle attach to the lateral plate of the pterygoid hamulus, a bony projection of the sphenoid bone. The lateral pterygoid muscle inserts on the anterior portion of the condylar neck. Contraction of these muscles moves the mandible forward (protrusion).
(9) is the mastoid process of the temporal bone. Muscles involved in tipping and turning the head attach at this point. (10) is the coronoid notch of the mandible, an important bony landmark when giving dental injections.
The TMJs are the only joints in the body that are partly rotational, and partly translational (the medical term for this is synthroathroidial). This means that for the first 10-15 millimeters of mouth opening (measured at the incisor teeth), the joints work like hinges—rotating around a stationary axis drawn between the two condyles. Opening the mouth further causes the condyles to move (or translate) down and forward, out of the glenoid fossae (Figure 2).
You can appreciate this by placing your fingers over the bony humps just in front of your ear holes. Open and close as wide as you comfortably can. You will feel the hump disappear as the mandible moves forward. By moving your mandible side to side with your fingers over the humps, you will really notice the movement as the mandible skews forward on one side and backwards on the other.
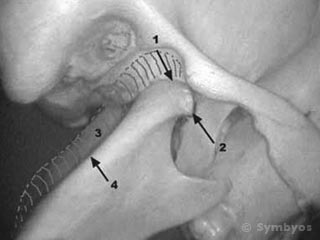
Figure 2: The mandible shown translated forward, with the condyle out of the glenoid fossa.
Figure 2 shows the open position of the TMJ. (1) is the area of entry of the retrodiskal tissues, where the nerve and blood vessel fibers enter the joint capsule. (2) is the lateral pole of the condyle, where the joint capsule ligaments attach. The joint capsule resembles a parachute, with the shock lines representative of the joint capsule ligaments.
Placing a finger over the lateral poles or in the ear and pushing forward gently with the teeth closed together will produce tenderness if there is inflammation in the joint capsules. The mandible is translated down and forward in the photograph. (3) represents the position of the posterior ramus of the mandible (4) when the jaw is closed.
Development of TMJ Dysfunction
Heavy muscle contraction forces in the jaw closing muscles (masseters, temporalis and pterygoids) can squeeze the cushioning disk. If this happens frequently enough, the disk can distort in shape. Part of it can squeeze forward into the joint compartment and part of it backward. Depending on which direction the bulk of it goes, either the opening path of the jaw can be interfered with, or the closing path. This can cause the jaw to lock either open or closed.
Even normal chewing muscle forces can damage the jaw joints if several of the back teeth are lost. This is because the back teeth help to reduce the amount of force experienced by the joints, by carrying a significant portion of the load.
Small, corrugated or irregular ripples that form in the articulating disk can cause clicking. Clicking can also be caused by ligament laxity, a stretching of the joint capsule ligaments that can occur with trauma or by forcing the mouth to open farther than normal. Distortion in the shape of the joint capsule is what causes popping. If the cushioning disk becomes perforated, a bone-on-bone situation like that shown in the Figures can result. Wear on the two bony elements can produce roughened surface osteophytes, bony projections which, when rubbing against each other produce grating (crepitus). This condition is known as TMJ arthritis.