Root canal therapy
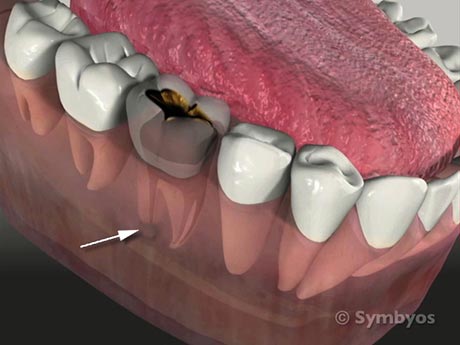
If infectious micro-organisms get inside your jaw bone, they can cause swelling and significant discomfort. Root canal therapy removes the micro-organisms, relieves pain, and seals the tooth against future bacterial invasion.
Root canal therapy is a procedure in which access to the hollow interior of the tooth is made, in order to remove inflamed, infected or non-living nerve and blood vessel tissue. The root canals are disinfected, enlarged and hermetically sealed to the root tips with a rubbery filling material. Finally, the access hole into the tooth is filled with any of the available filling materials like silver amalgam, composite resin, porcelain or gold (usually at a separate appointment).
Your dentist may recommend a dental crown (cap) following root canal therapy, especially if the tooth has multiple cusps or multiple roots, and is structurally compromised. Normally the front six teeth in both jaws only have single roots, and many times those teeth don’t need to be crowned after root canal therapy.
Root canal therapy is prescribed for teeth that have been diagnosed with an abscess, irreversible pulpitis, chronic apical periodontitis, inflammatory resorption or are necrotic (filled with non-living blood vessel and nerve tissue). Root canal therapy is also prescribed if the part of the tooth that is visible protruding through the gum tissues is badly broken down and would require structural posts to be placed in order to restore the tooth to normal function.
Sometimes a tooth that requires root canal therapy will be obvious from an X-ray image, if there are obvious changes in the bone near the root tip(s)—even in the absence of symptoms. Sometimes teeth with deep dental caries (cavities/tooth decay) require root canal therapy even though they may not hurt or be sensitive. A tooth that is particularly sensitive to hot temperatures, but is relieved by cold likely has gas from bacteria inside of it, most likely from an infection. Heating the tooth heats the gas, which, constrained by the hard shell of the tooth around it, cannot expand.
The result is that the pressure in the tooth increases and puts pressure on the nerve that you feel as pain. Teeth with such symptoms typically require root canal therapy to eliminate the infection. Teeth that produce continuous dull, achy pain frequently require root canal therapy. Teeth that have a prolonged, aggravated pain response to cold may need root canal therapy.
If you have been taking bisphosphonate medications, and require a tooth to be removed, you may not be a candidate for tooth removal without suspending the medication for a period of time in advance of treatment. In such cases, your dentist may recommend root canal therapy as an option, if it requires immediate treatment.
See also on ToothIQ.com