Dental caries (cavities/tooth decay)
What are dental caries?

Figure 1: A scanning electron micrograph of a colony of Streptococcus mutans bacteria, such as those found in the fuzzy plaque on teeth. These are the bacteria responsible for the vast majority of tooth decay. (Image from http://www.zahnarzt-stuttgart.com, used with permission).
Dental caries is a bacterial illness believed to be caused by a single strain of bacteria known as Streptococcus mutans, although Lactobacillus may also be involved. These bacteria use sugars from the food and drinks we eat, to produce acids and enzymes that attack tooth enamel.

A sugary diet and poor oral hygiene results in tooth decay (caries).
Directly consumed acids, such as phosphoric acid found in many soft drinks, can also attack tooth enamel, resulting in the decay of the tooth. Food and drink containing citric acid (for example, lemons) should be consumed in moderation.
Tooth decay can devastate teeth, even with all that is known about its causes, and all of the excellent preventive measures available to stop the disease. Proper nutrition and excellent oral hygiene are the keys to avoidance of tooth decay.
How does the dentist diagnose Tooth Decay?
Note: ToothIQ.com contains general information. Only a dentist can properly diagnose your specific condition.
Traditionally, dentists have detected tooth decay in one of three ways: visual and tactile examination; and dental X-ray images.
Visual/Tactile Exam
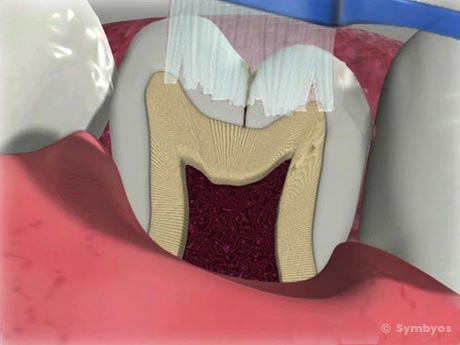
Pits and fissures in teeth may be too deep and narrow to allow access for even one toothbrush bristle, as illustrated by this cross section of a tooth.
Some tooth decay is visually obvious; other tooth decay may develop in the deep pits and fissures of teeth. Some studies suggest as many as 80% of tooth decay begins in pits and fissures.

Dental explorers have been used for many years to detect early tooth decay.
Dentists typically use an instrument called a dental explorer, a sharp, wiry instrument for probing the depths of the pits and fissures. If the base of the pit or fissure is softened by tooth decay, the instrument will stick in the tooth.
X-ray Images

Tooth decay has occurred where an impacted wisdom tooth (third molar) has been leaning against a second molar tooth (See arrow). Without the dental X-ray image, the decay would have gone undetected.
Tooth decay is visible as dark areas of the tooth on dental X-ray images. Dentists use dental X-ray images to look for tooth decay where a visual/tactile examination is not possible, most notably between the teeth.
Tooth Decay Detection By Laser

An artist’s rendering of the tip of a laser fluorescence tooth decay detection meter emits a focused beam of 655nm wavelength light into the pits and fissures, causing fluorescence of decayed tooth structure. The amount of fluorescence is directly related to the extent of the tooth decay. Healthy tooth enamel does not fluoresce.
An extremely sensitive diagnostic tool for determining whether the pits and fissures in teeth have begun to decay at their base is the laser fluorescence caries detection device, the tip of which is shown in the image below.
Healthy teeth do not fluoresce, and decayed teeth fluoresce in proportion to the amount of bacteria present in the tooth. This device measures the fluorescence pattern of teeth, and produces a reading on a meter which is recorded by the dentist.
Diagnosis of pit and fissure cavities is most effective when a combination of visual/tactile examination, appropriate use of laser fluorescence caries detection devices, and X-ray images are used.
How is Tooth Decay treated?
Depending on the severity of the decay, restoring teeth with tooth decay may involve fillings, inlays, onlays, dental crowns (caps) or tooth extraction. Tooth decay that reaches the inner pulp of the tooth may require root canal treatment to eliminate the bacteria. Sometimes early decay can be slowed down or stopped by applying topical fluoride to the affected area. Photographs and dental X-ray images are useful for monitoring tooth decay.
Recurrent Caries
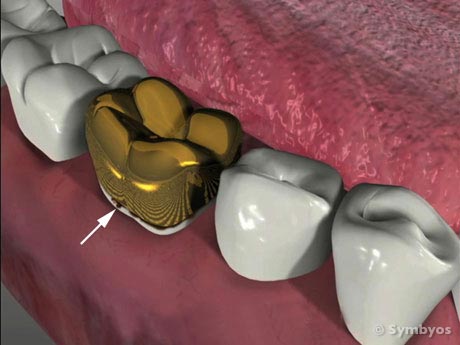
Recurrent caries (tooth decay) at the margin of a gold crown. It is a potentially costly mistake to think that teeth which are covered with crowns cannot decay further.
Recurrent caries is tooth decay that occurs under existing dental restorations, such as fillings, crowns, or onlays. It may be caused by poor oral hygiene, or by development of a microscopic pathway for leakage (micro leakage) past the dental restoration.
Micro leakage allows acids and bacteria access to areas of the tooth that are not accessible to toothbrush bristles or other oral hygiene aids.The possibility of micro leakage is a strong motivator for replacement of questionable dental restorations, as well as complete removal of old restorative materials (for example, core buildups and bases) in a tooth that will be receiving a new crown or onlay.
See more on ToothIQ.com