Oral Habits of Children
Many children place fingers, thumbs, pacifiers or blankets in their mouths to provide them with a sense of emotional comfort and security. These habits can result in irregular positioning of the teeth, and may negatively influence the development and positioning of the jaw bones, especially the upper jaw (maxilla). They can also affect the early development of speech.
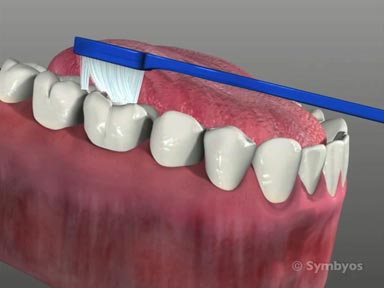
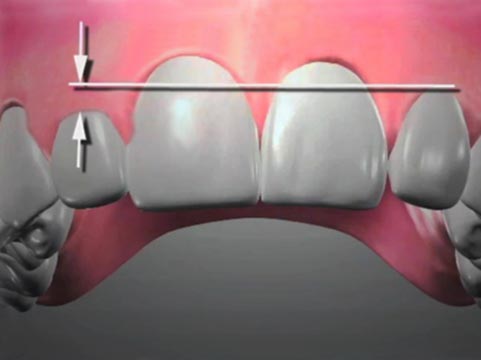
Long-term application of suction causes the cheeks to place inward pressure on the upper teeth, which ultimately leads to a narrowing of the palate (palatal constriction), reverse overlap of the upper and lower back teeth (posterior crossbite), and an outward flaring of the child’s upper incisor teeth (incisor protrusion). Often the lower incisors will tip toward the tongue as well (incisor retrusion). This increases the child’s overjet—the horizontal distance by which the upper incisors overlap the lowers, and increases the likelihood of the child chipping or otherwise injuring a front tooth.
Because such children spend a significant amount of time with objects between their front teeth, the back ones frequently erupt farther than normal (passive eruption). When this happens, the child’s front teeth may no longer overlap vertically, a condition known as an anterior open bite. The child’s speech development may be affected in such cases, as well as their ability to chew properly.
Children may also habitually position the tongue against the front teeth (tongue thrusting), rather than resting it against the palate. This can lead to outward flaring of the front teeth, irregular swallowing and phonetics concerns. Re-training of the tongue muscles through appropriate exercises may be needed prior to orthodontic treatment.
More on ToothIQ.com