Tooth extractions
Tooth extractions typically fall into two categories: “simple” and “surgical.”
Simple tooth extractions
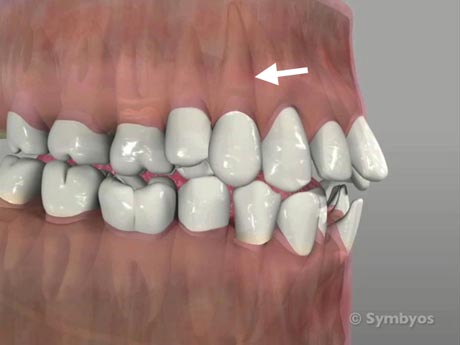
Teeth that have straight roots (see arrow) are generally the best candidates for simple tooth removal. They should also possess a tooth structure that is solid enough for the dentist to use dental instruments to grab and manipulate the tooth.
Simple tooth extractions are tooth removal procedure that can be accomplished from above the gums using traditional elevator and forcep instruments. It is a process of removing teeth without the need of surgical techniques, which are called surgical tooth extractions.
Generally, teeth that are candidates for simple tooth extractions have straight roots and enough solid tooth structure extending through the gums to grasp and manipulate with the instruments. “Simple” implies that the tooth is not cut into pieces and no incision is made in the gum tissues to gain access to the tooth.
Simple tooth extractions are prescribed if teeth are too extensively damaged from decay or trauma to be fixable, or if they are infected and the patient is not a candidate for root canal therapy. Simple tooth extractions are also frequently prescribed when the teeth in one or both jaws are severely crowded, and straightening the teeth would require unnecessarily complex orthodontic treatment with a compromised treatment outcome. Most commonly, either two or four bicuspid teeth are removed in cases of significant crowding.
Sometimes the decision to remove a tooth is based on cost, if the procedures required to restore it would involve significant expense. This is especially true if the likelihood of long-term success is not good.
Surgical tooth extractions
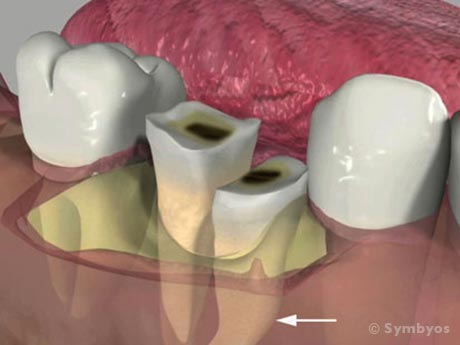
Figure 1: A non-restorable lower molar tooth with a curved (dilacerated) root is less traumatically removed if the tooth is divided into pieces. Whether or not a surgical access flap is required to do this, the procedure is considered surgical if the tooth is sectioned into pieces.
Surgical tooth extractions are tooth removal procedures in which surgical access is required to completely remove a tooth. Even if the tooth is visible in the mouth without surgically exposing it, surgical techniques may be necessary to remove the tooth. This includes sectioning the tooth into two or more pieces, whether or not a soft tissue incision is made. Surgical extraction does not necessarily mean that the dentist removing the tooth has advanced training in oral surgery, and you will generally not be billed for surgical tooth extractions unless the tooth is sectioned into pieces, or an incision into soft tissue is made. Surgical tooth extractions include removal of impacted wisdom teeth (third molars), but this does not mean that all wisdom teeth requiring removal are required to be removed surgically.

Figure 2: A soft-tissue impacted lower wisdom tooth (third molar). Removal of this tooth is also less traumatic if the tooth is divided into pieces. Often, impacted teeth require a surgical access flap to be made in order to provide better visibility for the dentist.
Removal (extraction) of a tooth is prescribed if the tooth is too extensively damaged from decay (Figure 1) or trauma to be fixable, or if it is infected and the patient is not a candidate for endodontic (root canal) treatment. It is also frequently prescribed when the teeth of one or both dental arches are severely crowded, and straightening the teeth would require unnecessarily complex orthodontic treatment with a potentially compromised treatment outcome.
Most commonly, either two or four bicuspid teeth are removed in such cases, and generally they are removed by “simple”, not surgical technique. Sometimes the decision to remove a tooth is based on cost, if the procedures required to restore it would involve significant expense. This is especially true if the prognosis for the tooth (i.e. likelihood of long-term success) is not good. Wisdom tooth removal is frequently recommended, and ideally prescribed in the late teens to early twenties, if it is apparent that these teeth will not fit in the jaws in a normal bite relationship with normal gum tissue contours.
Extensively damaged teeth, and teeth with multiple curved roots frequently require extraction by surgical technique when removal is necessary. Teeth which have been endodontically treated and later need to be removed for some reason, frequently require surgical technique as their roots tend to be more brittle.
See more on ToothIQ.com